Drug resistant fungi
Solving the next big threat to humanity
Our UVC is your front-line in defence.

We know the right wavelength of UVC light effectively kills Covid. UV light also kills moulds, bacteria and fungi, which is very good to know because one of the biggest threats to human health is killer fungi. They're resistant to the usual treatments, and they're on the increase. Here's what you should know.
Antibiotic resistant fungi are developing at an 'unprecedented pace'
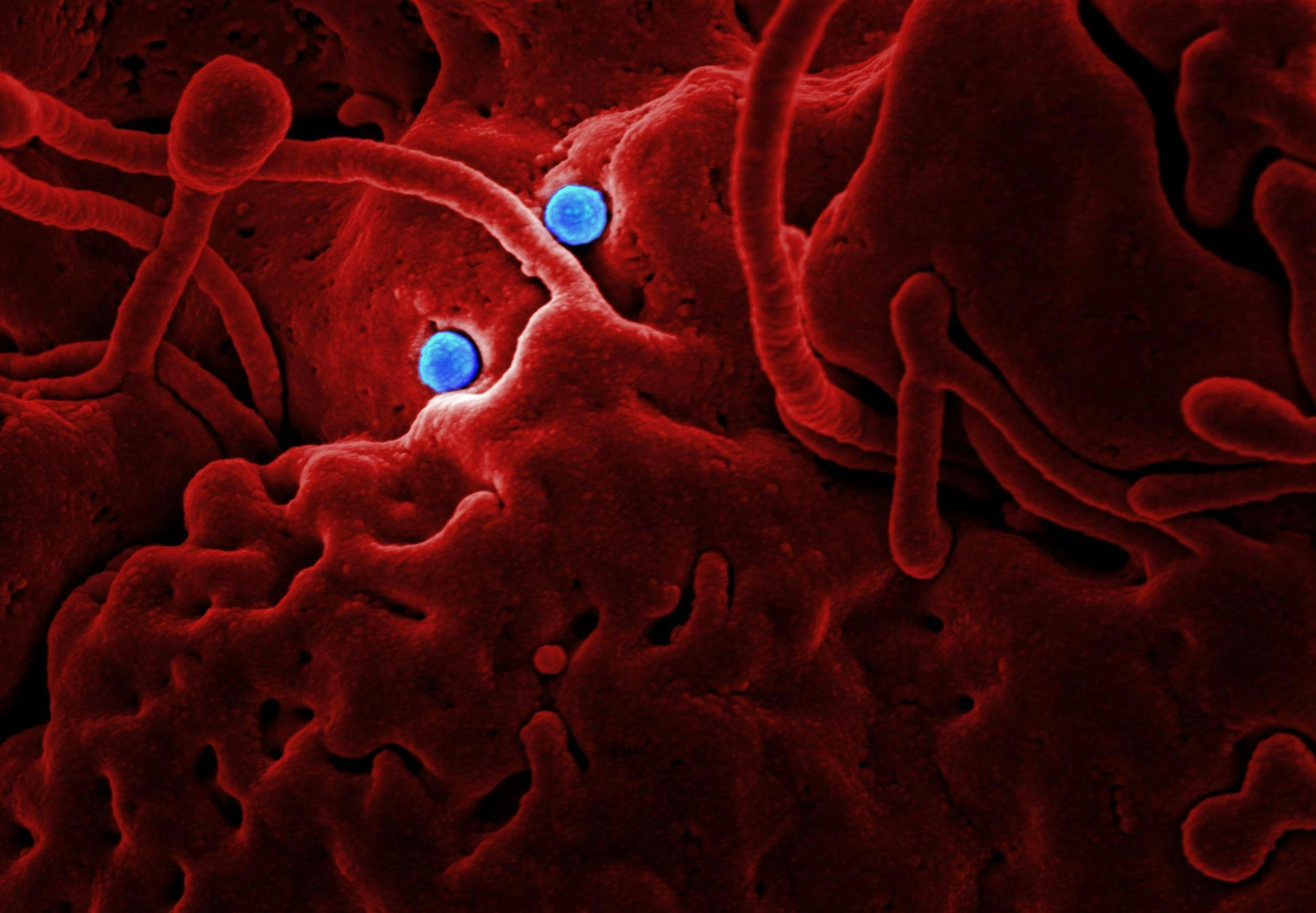
While thousands of different fungi live with us and inside us without causing any harm, some of them can spread deadly infections.
Every year millions of people in hospitals around the world catch infections that prove more dangerous than the illness that sent them to hospital in the first place. Methicillin-resistant Staphylococcus aureus, also called MRSA, and Clostridium difficile, both shrug off antibiotics with ease. But they're only the tip of the iceberg.
Diseases like pneumonia, tuberculosis sepsis and gonorrhoea are also becoming more of a challenge to treat thanks to growing antibiotic resistance. But treatment-resistant fungal infections are the latest kid on the block, and they're incredibly nasty. So far 90% of worldwide outbreaks in hospitals have been down to Candida auris, which is often resistant to humanity's best antifungal treatments.
Worst of all, fungal resistance is developing at an 'unprecedented pace' and it isn't restricted to hospitals. Resistant fungi are popping up in the air we breathe, in the soil, all over the place.
About anti-fungal treatments
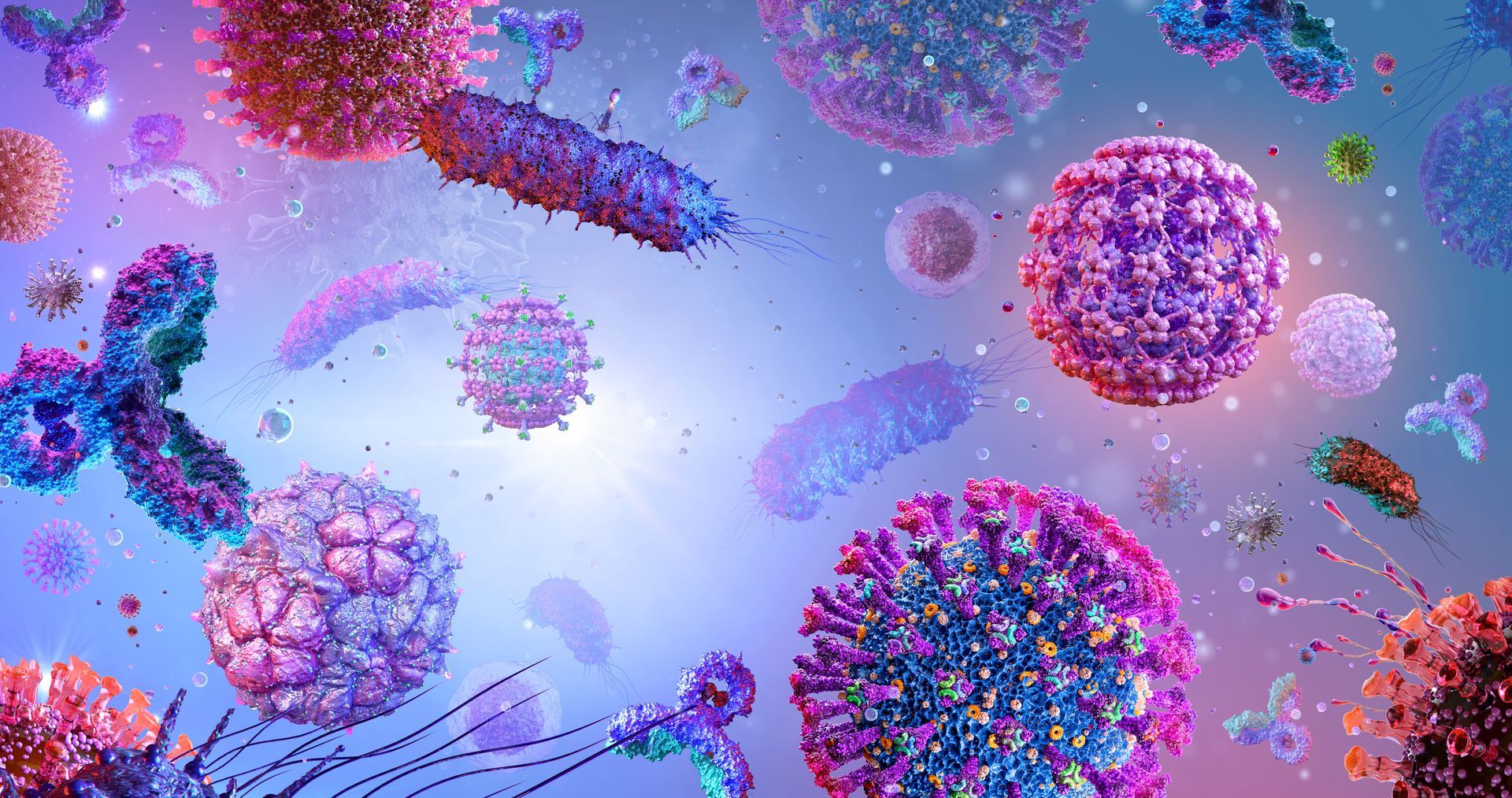
There was no such thing as a reliable anti-fungal treatment before 1950. The late 1960s saw new drugs called azoles arrived, killing fungus by disrupting their cell membranes. Triazoles followed in the late 1980s, giving the human race a choice of antifungal medicines with fewer side effects. These days we tend to use either triazoles, amphotericin B, or echinocandins to treat people who can't fight off fungal infections on their own.
Luckily fungi are not very good at efficiently transmitting between people. But one of them, C. auris, is now present in hospitals on six continents and most strains of it are resistant to at least two of the three treatments we have on hand. This is a very scary beast, named “almost the perfect pathogen,” by Johanna Rhodes, a genomic epidemiologist at Imperial College London. It can hang around on inanimate surfaces for as long as 28 days and resists all attempts to kill it off. It first turned up in the UK during 2015, and early 2019 saw more than 260 UK cases. The USA has had over 1000 cases so far and there have been large outbreaks in Spain, Venezuela, Colombia, India and Pakistan. If the C. auris infection gets into the bloodstream, it will kill more than 33% of people within weeks.
The incidence of treatment-resistant fungal infections is rocketing. One Dutch study revealed azole resistance in some fungi almost doubling between 2013 and 2018. And in 2019 just under 7% of A. fumigatus fungi found in soil samples in the south of England tested positive for azole resistance. The same goes in Europe, the Middle East, South-East Asia, the US, Colombia, Australia and Tanzania. In 2015 – 2018 Candida glabrata became more resistant to three different antifungal drugs. And fungal pathogens like Scedosporium and Fusarium, both common in soil, are also steadily becoming resistant.
The cause of all this increasing resistance isn't always clear but climate change has been tipped as an important factor. Take C. auris, which thrives at higher temperatures than related species. Some say the fungus is adapting fast to warm environments because of climate change. The broad use of azole-based fungicides in agriculture isn't helping. And many researchers believe resistance is growing thanks to the widespread use of triazoles in hospitals, which creates an 'open ecological niche for C. auris' and leads to 'restructured fungal populations' that are more likely to affect humans.
How are the world's scientists responding to the fungal threat?
The world is responding with several large studies into fungal resistance. Experts are recommending placing greater restrictions on fungicides, including selectively withdrawing some azole-based fungicides from farming. We also need new antifungal drugs, which is actually quite hard to create since humans are more closely related, genetically, to fungi than we are to bacteria, which means anti-fungal treatments are also toxic to humans. Ironic or what!
Two drugs, ibrexafungerp and rezafungin, are being tested in large trials at the moment. Another, olorofim, works by blocking the production of pyrimidine, a precursor of DNA. More new drugs are under development, but it could be at least five years before they're ready for use. When they are released, experts say they should be used for medicines, not harnessed for farming. There's a lot of work going on around RNA interference, too.
UVC does the trick
While drug-resistant fungal pathogens aren’t making headlines yet, they're predicted to do so. This means we need to spend more on plans to deal with all types of infectious diseases in the future. In the meantime, our UVC LED technology is an exceptionally reliable way to kill off fungi as well as viruses, bacteria and moulds. If you want to protect your business from future threats, UVC light is your front-line defence.